Trauma Isn't What Happened — It’s What Happened Inside
Trauma isn’t the event itself.
It’s the internal experience—the meanings your mind made, the threat your body registered, and the protective patterns that formed to keep you safe. And while trauma is never your fault, recovery becomes your responsibility — the moment you take your power back.
TABLE OF CONTENTS
What Trauma Really Is (and Isn’t)
Common Myths
How Trauma Forms in the Brain & Body
Types of Trauma
Signs & Symptoms
“Not Your Fault, But Your Responsibility”
Evidence-Based Ways to Heal
Rapid Transformational Therapy (RTT) For Recovery
FAQs
What Trauma Really Is (and Isn’t)
Trauma is a nervous system and the mind's meaning-making response to something that felt like “too much, too fast, too soon—or for too long—without enough support.” Two people can live through the same event; yet one is shaken but resourced, while the other carries an internal imprint that shapes thoughts, emotions, and behavior. The difference isn’t character — it’s capacity, context, and support.
- Event vs. Experience: the incident is external; trauma is the internal imprint.
- Threat over facts: your body encodes perceived danger, not just the objective details.
- Protective, not pathological: survival responses (fight, flight, freeze, fawn) are intelligent adaptations that can be updated. They are responses to the perception of danger (real or imagined) and are not fixed.
Common Myths Debunked
❌ Only extreme events cause trauma.
✅ Everyday experiences (neglect, chronic criticism, medical procedures, identity-based harm) can be traumatic.
❌ If it was traumatic, I’d know immediately.
✅ Responses can be delayed or dissociated to protect you.
❌ Trauma always means PTSD.
✅ It may appear as anxiety, depression, relational patterns, or body symptoms without meeting PTSD (Post Traumatic Stress Disorder) criteria.
❌ Time heals all wounds.
✅ Time with safety, support, and repair heals, but unprocessed trauma tends to repeat in patterns.
❌ Therapy is one-size-fits-all.
✅ People heal through different ways and approaches — somatic, cognitive, relational, and subconscious work.
How Trauma Forms in the Brain & Body
- Amygdala (alarm) tags danger fast.
- Hippocampus (timeline) can go offline—memories feel present-tense or fragmented.
- Prefrontal cortex (reasoning) dims under threat; it’s hard to “think your way out.”
- Autonomic nervous system shifts into survival states: hyperarousal (fight/flight), hypoarousal (freeze/collapse), or fawn (appease).
- Meaning-making locks in: “I’m not safe,” “It was my fault,” “My needs are too much.” Healing updates these implicit beliefs.
Types of Trauma
Acute: a single incident.
Chronic: repeated stressors (e.g., ongoing conflict, caregiving strain).
Complex/Developmental: prolonged exposure, often in childhood or attachment relationships.
Vicarious/Secondary: absorbing others’ trauma (common for leaders, clinicians, founders).
Collective: community-wide events (e.g., natural disasters, displacement of home, political systemic oppression, etc.).
Signs & Symptoms
These are protective strategies your system learned. Recognition is the first repair.
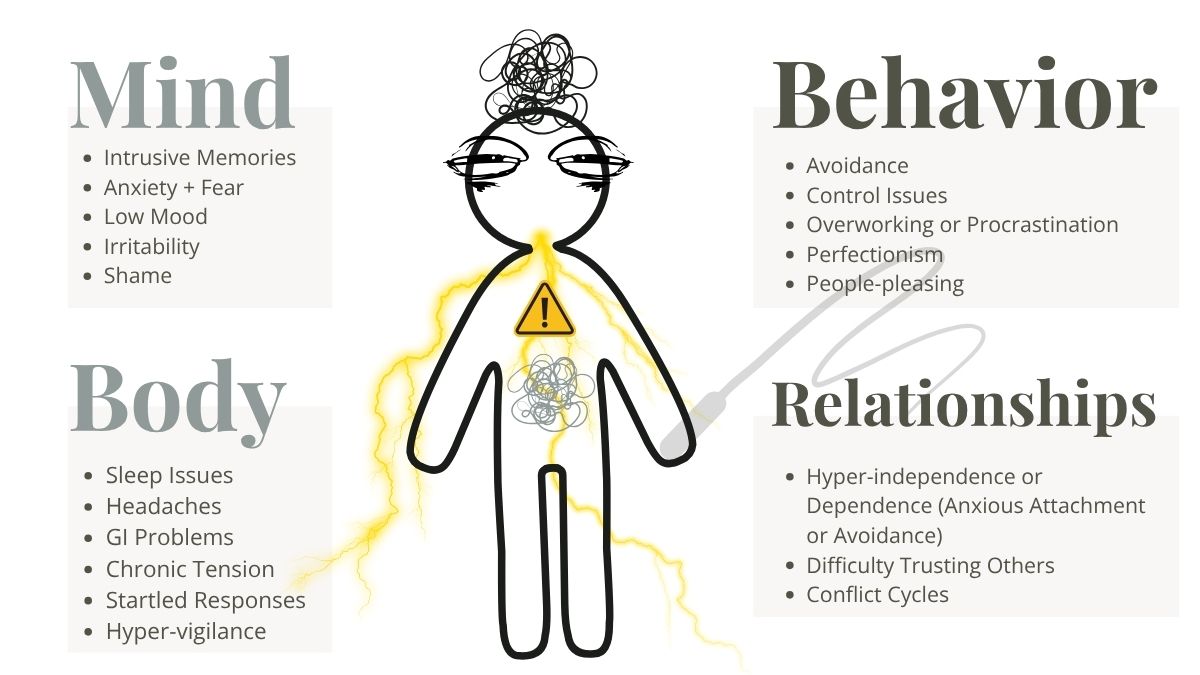
- Mind/Emotion: intrusive memories, anxiety, low mood, irritability, shame, perfectionism.
- Body: sleep shifts, headaches, GI issues, chronic tension, startle response.
- Behavior: avoidance, overworking, procrastination, control patterns, numbing, people-pleasing.
- Relationships: hyper-independence or dependence, trust difficulties, conflict cycles.
“Not Your Fault, But Your Responsibility”
Blame keeps you stuck; responsibility restores choice.
Responsibility here means response-ability — the capacity to meet what arises with tools, support, and self-leadership.

- Acknowledge: what happened wasn’t okay—and it wasn’t your fault.
- Resource: build safety (body up) before processing story (mind down).
- Repair: update old meanings with present-day truth and support.
- Reclaim: choose boundaries, rhythms, and relationships that protect your energy.
Evidence-Based Ways to Heal
There's no one-size-fits-all approach to healing trauma.
The best approach for you depends on your type of trauma and symptoms (what you are struggling with specifically). A multi-layered approach is often beneficial.
Bottom-Up (body first)
-
Breath pacing (longer exhale), orienting, vagus-nerve stimulation, rhythmic movement, gentle cold/warm contrast, sensory grounding.
-
Somatic therapies (e.g., SE), trauma-sensitive yoga, EMDR’s bilateral stimulation.
Top-Down (mind + meaning)
- Trauma-focused CBT, RTT, parts-work/IFS-informed approaches, compassionate reframing of core beliefs.
- Narrative repair: witnessing your story in a safe relationship.
Relational Repair
- Co-regulation, attachment-aware boundaries, group/community healing.
Subconscious Repatterning
- Hypnosis-based methods help access and update beliefs laid down during threat so that behavior can change with more ease.
Daily micro-practices (5–10 minutes)
Name + Notice + Nurture
→ Name the state, notice body cues, nurture with one regulating action.
1% Safety Shift
→ Do one tiny behavior that signals safety (drink water, open a window, step outside). It pays compound interest.
Future-You Rehearsal
→ Visualize one aligned boundary or conversation that would typically trigger you while staying regulated.
Rapid Transformational Therapy (RTT) For Trauma Recovery
You didn’t choose what happened. But you can choose what happens next.
Healing is re-learning safety, rewriting meaning, and returning home to yourself.
RTT combines hypnosis with targeted CBT-focused therapeutic tools to access the subconscious, uncover the meanings formed during the original experience, and reframe limiting beliefs with accurate and compassionate truths.
Clients often notice:
- Reduced reactivity and shame, more emotional range and capacity
- Clearer boundaries and reduced people-pleasing or perfectionism
- Increased capacity to follow through on supportive habits.
If you’re ready to free yourself from old meanings that are keeping you stuck and rebuild from inner safety, explore Rapid Transformational Therapy (RTT).
FAQs
Is trauma the same as PTSD?
→ No. PTSD (Post Traumatic Stress Disorder) is one possible outcome. Many people carry trauma patterns without meeting the clinically diagnosable PTSD criteria. It involves persistent, severe symptoms lasting longer than a month that interfere with daily life.
Can I heal without talking about the details of what happened?
→ Yes. Somatic and subconscious work can reduce activation without you needing to re-tell the whole story. It's your interpretation of what happened and the meaning that needs reframing; that's what creates healing.
How long does trauma last?
→ The duration of trauma and recovery varies widely depending on the type and severity of trauma, individual factors, and access to support. Trauma unfolds over time—from an acute stress reaction immediately after the event, through weeks to months of emotional and physical symptoms. If symptoms persist beyond a month and impair daily life, this may develop into PTSD, which often requires specialized treatment. Symptoms can last from days to many years, depending primarily on trauma type, individual resilience, and treatment received. Early intervention and supportive care improve the speed and quality of recovery.
Why do I feel “fine” and then suddenly feel flooded?
→ That’s state-dependent memory — when your body enters a similar state, stored material becomes vivid.
How do I support someone I love with trauma?
→ Prioritize safety and consent. Listen, don’t fix. Ask what helps their body feel calmer in the moment.